|
sWhile I am tempted to reflect on how utterly impossible this past year and half has been - I am going to forego that impulse to reflect on a moment of grace and time spent, quite literally, in the golden hour.
A perfect hour - warm breezes after months of triple digit heat, air cleared by a freak rainstorm after weeks of smoke laden AQIs, and the beauty of the mountain literally glistening gold in the light. I think of Tanizaki's writings - Praise to Shadows and his appreciation of nuance as a form of mindfulness. "Junichiro Tanizaki selects for praise all things delicate and nuanced, everything softened by shadows and the patina of age, anything understated and natural—as for example the patterns of grain in old wood, the sound of rain dripping from eaves and leaves, or washing over the footing of a stone lantern in a garden, and refreshing the moss that grows about it – and by doing so he suggests an attitude of appreciation and mindfulness, especially mindfulness of beauty, as central to life lived well." I suspect the beauty of these moments of light is made more poignant because of the months, and continued threats, of darkness.
1 Comment
Dear Mermaid Family:
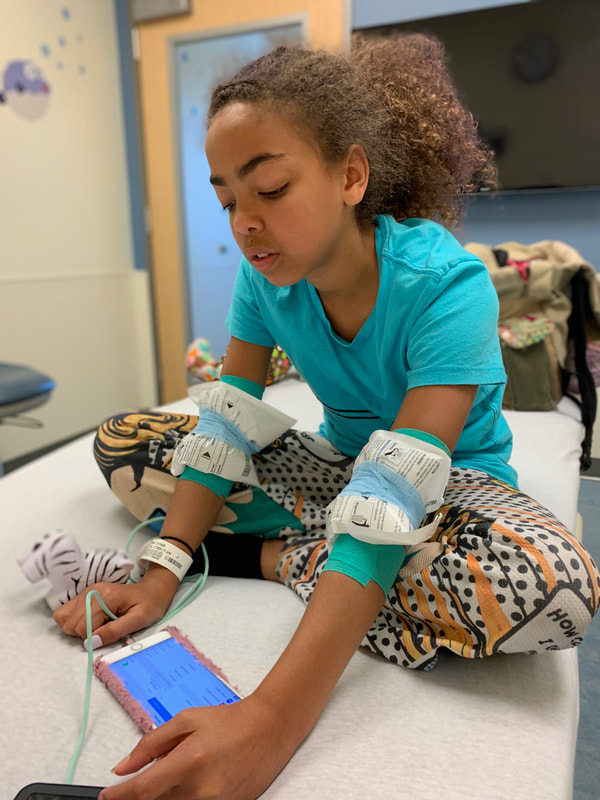
Please break your quarantine to take your immunosuppressed child and her asthmatic caregiver to a place where people are known to have COVID-19. You will share a garage and those tiny elevators with people who have COVID-19 with your medically fragile, asthmatic child. You will wait outside in a group, asked to disinfect your hands, and then will be given a face covering that may or may not be effective against viral transmission. Then you will be asked to go sit for up to seven hours in an unventilated room filled with people who you are told are "asymptomatic" who may or may not have been following sheltering in place orders. Who may or may not have had the privilege of living in the total isolation your family has been in for the past 43 days. And who may or may not be shedding the virus. The only thing that is certain is that you will do this without PPE that has been proven effective against viral transmission. You will share sinks, bathrooms, water faucets, outlets, chairs, and other high hard contact surfaces that will not be cleaned between uses. You may be required to sit less than six feet apart from people you do not know. You will be asked to trust that it will be "OK". You will be told you are doing the right thing. We understand that you are aware that there are empty rooms that could be repurposed to minimize exposure. In other words, there are resources to mitigate and minimize your exposure to COVID-19 . We will not be offering those to you. We hope you will feel safe when you are with us and that you will trust we are doing our best for your family. My daughter Lala (12) has a rare disease that requires her to get regular (chemotherapy-like) infusions at UCSF. These infusions take between 5-7 hours and are necessary to keep her health stable. However, the pediatric infusion area at UCSF (Mission Bay) is not practicing social distancing (I have been told there are times when each chair may be full - putting patients within close proximity to one another) and creating a number of risks, which are detailed below. Requests to secure a private room have resulted in a “that may not be possible”.
My daughter is getting sicker - and I have delayed her treatment longer than is wise or medically advised trying to advocate for changes in infusion center practice. The irony is our greatest risk of catching Covid-19 is getting treatment for Lala’s underlying health condition. We have been in total isolation for 40-days. And though all other communal spaces are closed and social distancing is mandated throughout the medical center and hospital- the public infusion bay is still open with chairs placed in some cases less than six feet apart for treatments that run up to 7 hours separated by “privacy curtains”. There is an intention to not fill the infusion bay, but there are no guarantees offered to patients that the PIC won't be completely full. Not all of the high contact surfaces are cleaned between patients -bathrooms, doors, faucets, outlets, visitor chairs, etc. I have been told if it will make me more comfortable I can disinfect the surfaces used by other patients that my daughter comes into contact with. Now let’s talk about PPE or the lack of meaningful versions of it. There are no aprons, visors, N-95s, etc for the nurses who move from patient to patient because it assumed by the medical center that everyone is COVID negative on the unit. Something we are asked to not assume in other public spaces. In the past, during visits to the same infusion center, when I have had a suspected cold or virus or a staff member has had the same- everyone has practiced droplet isolation. I have been covered head to toe in Tyvek/masks/gloves/etc. and the nurses gown up, wear PPE (masks, glasses, etc), and change each time they come into contact with my daughter and before working with another patient. I am perplexed why that is not happening now in a moment in history where it is prudent to assume we are all potentially infected with COVID-19. Nurses are not wearing n-95s unless patients are symptomatic - of which none are in the infusion center. And while patients and providers are wearing face coverings; the science behind non-N95 masks preventing viral transmission is not well established. I wonder why UCSF is not erring on the side of health and protection of its most vulnerable patients? My concerns have been met with regular responses from the medical center that no one with symptoms is allowed in the infusion center and that children are not getting infected with Covid-19. Unfortunately, new studies show that our children may not be as protected as we had thought. A study just published in the Journal of Public Health Management and Practice looked at data between March 18-April 6. During that time, 74 children were admitted to the PICU for COVID-19 across 19 states - 30% were children < 2 years, 24% 2-11 years, and 46% 12-17 years. Based on epidemiologic calculations, the researchers estimated that for each child who requires intensive care for COVID-19, there are 2,381 children infected with SARS-CoV-2, which means that approximately 176,190 children were infected with the virus during that 3-week period. The Chinese CDC has also published recent studies showing higher rates than originally thought among children. And recent research conducted by Stanford and other medical centers indicate that far more people are asymptomatic carriers than originally thought. I, like many other parents of children with rare diseases right now, am having to choose between depriving my daughter of a critical treatment, or putting both of my medically fragile kids at risk from the virus. There are some relatively simple changes that could make a huge difference in risk factors for Lala and other kids. This is not an abstraction - my sister was infected with COVID-19 during a recent infusion at a well respected research hospital in NYC. I am asking for the following changes: 1. All families seeking infusions be offered the use of a private room with its own bathroom; or a private room with the use of a bathroom that is professionally disinfected between each use (only in the case of emergencies should public infusions areas be used while maintain strict social distancing); 2. All families/staff be offered the option to use PPE and the protocols offered for droplet isolation in the infusion center; 3. All families seeking infusions be offered a "cold" or entrance/elevator separate from the areas screening people with suspected respiratory infections; 4. All families be offered a "side" of the garage that designated for immunosuppressed kids (so designated elevator) and protective equipment (facial covering) prior to entering the elevator. Home infusion is not an option because of insurance. We cannot be assured of a private room in the infusion center. We cannot be assured that the public bay won't be at capacity. There are good intentions but few commitments. I know that there are empty hospital rooms, open because of canceled non-essential and elective procedures, that could be used to infuse in privacy & safety. Rooms that would offer more protection for patients and staff. As of yesterday following a conversation with the infusion center charge nurse (who is amazing and does not make policy), my choice is risking the public infusion bay (there is no way to tell if it will be crowded or not) or letting Lala’s health take a dangerous turn. I worry as the only adult (an asthmatic one) in our household of medically fragile former foster children, what will happen to the girls (also asthmatic) if I get sick? What if they get infected? How I can quarantine Lala and I apart from my other 13 year old daughter when we get home from the medical center in a way that is humane and feasible while caring for the health needs of both kids? Sure I will do all the decontamination protocols and do my best to keep us safe - I just believe that the medical center can and should do better in protecting its most vulnerable patients and their families. I am asking for things that prior to COVID-19 were available in the PIC to patients with concerns about viral infection. I have faced many challenges as the mother of medically fragile children, I have had to make many hard decisions regarding their care, but never before have I knowingly put them in the path of avoidable harm. Please help me by doing what you can to insist that the pediatric infusion center make every effort, even the inconvenient ones, to reduce the risk to vulnerable children during the COVID-19 pandemic. So the reality of today's medical center visit was not so terrible - its just six hours... I think its the relentlessness of the illness- it's constant demands for attention that wear... bc we had been sick (and by we- I mean all three of us) we were placed in infection control (so many glamorous masks/gowns/booties/caps/gloves) --
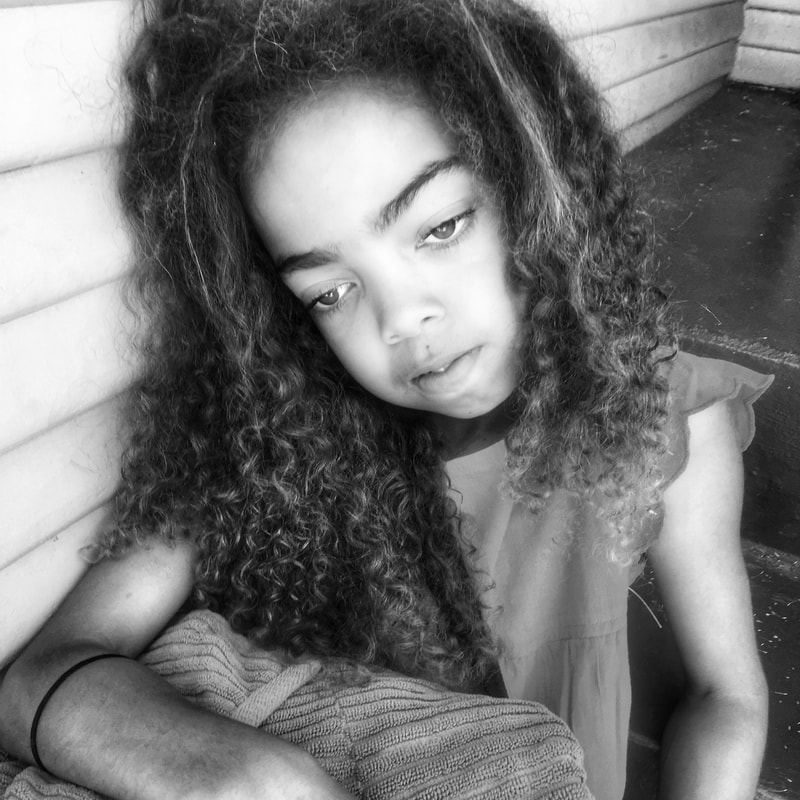
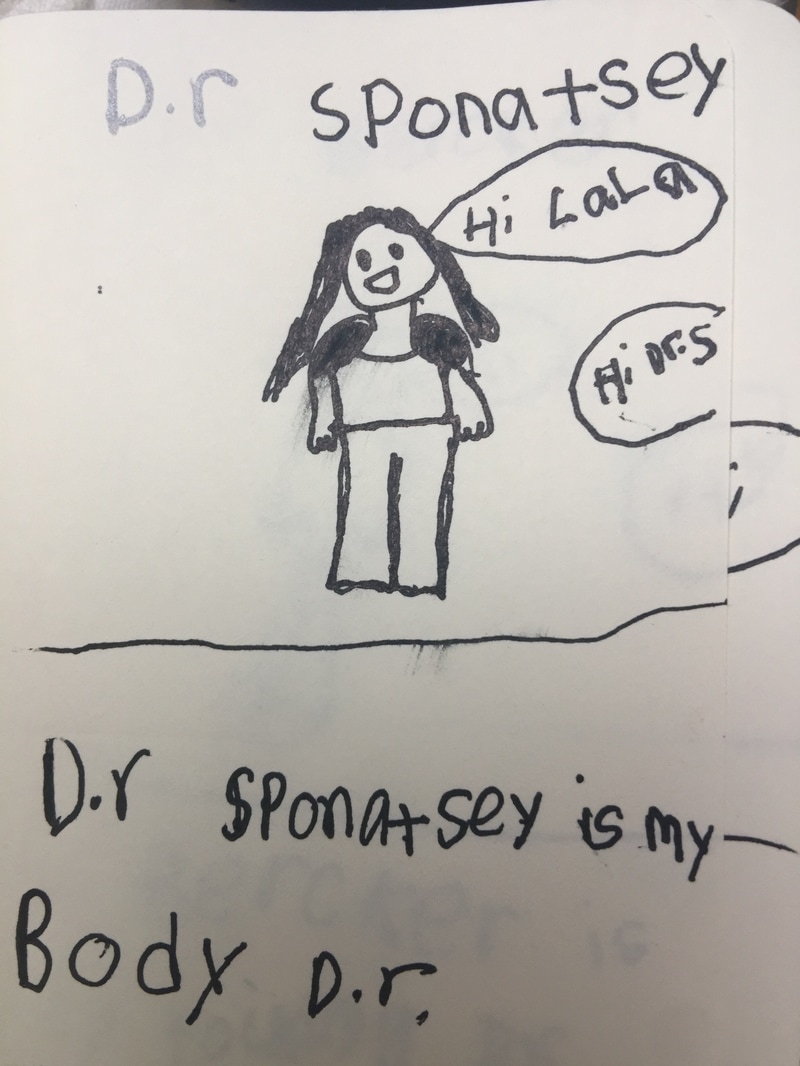
I packed sushi, a birthday cake, the worst popcorn in the world, games, and - of course- knitting. I let the kids have unlimited screen time, we sang Stevie Wonder songs, I billed client time, Lala created a unicorn rebel avatar, I didn't cry when Lala did bc of the needles, Sarah pondered (she is such a bad ass) on the whole focus on unicorns being white not black, and drop by infusion drop we passed the hours ... until it was time to uber home. Everyone was wonderful - the pediatric infusion center is the best of the best - and I feel so grateful for their care for Lala that I could weep. They are so patient centered. They honor Lala as the individual she is and they believe in choice and kids being in charge of their own bodies. It makes me weepy bc its so uncommon in this system of medical care. The body is not an apology - and there is so much work to be done if you happen to be a female, child, person-of-color, who is not able bodied. At the end of the infusion- we all sat on the bed with the best-nurse-ever (Stella) - and shared pictures and stories about our silly little dogs -- #winning - Lala was not psychotic from the medication this time so the uber home was uneventful. There is a gender divide in medicine when it comes to how pain is seen, treated, and perceived in women patients. I am familiar with and write about racial bias in pain management - I was not prepared for the presentation of the intersectionality of medical racism, and the sexism, in the form of under-diagnosing and under-treating my 10 year old bi-racial daughter's pain. Nor was I prepared for or willing to accept that anxiety, hers or mine, was the cause for her pain when she has a diagnose for IBD, Chron's Disease, and an undifferentiated Systemic Autoinflammatory Disease that causes objectives measures of pain (lesions, elevated SED/CRP levels, visible inflammation, etc.) that measure 10/10 or the crying face on the pediatric pain scale.
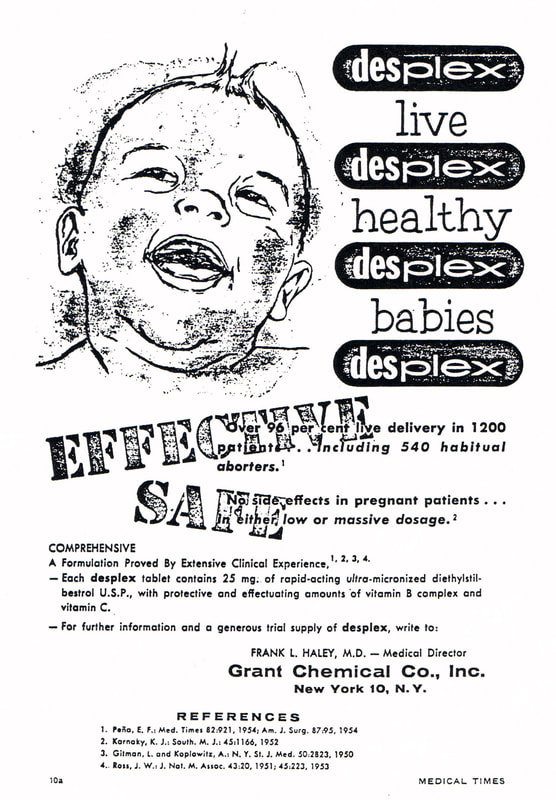
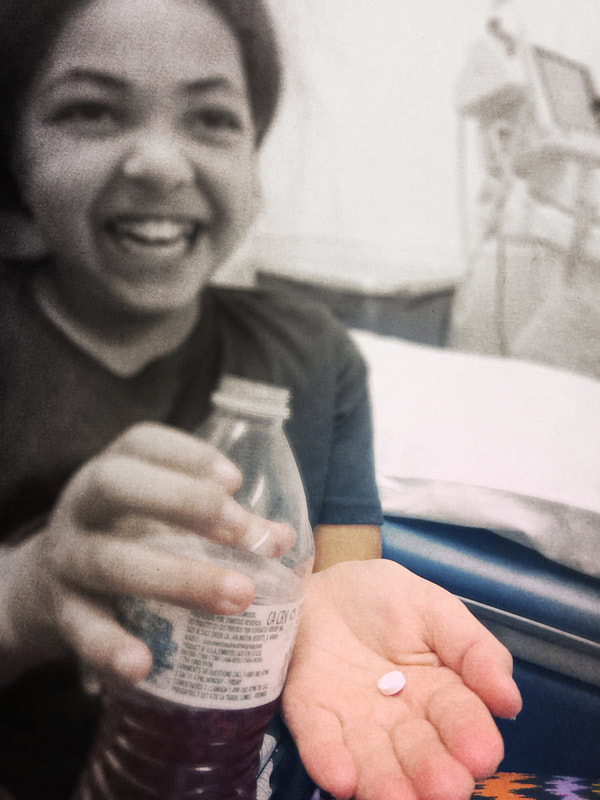
Being female, being bi-racial, being a child, and having a rare disease is a recipe for under-management of pain and doubting of symptoms. And with that under-management of chronic pediatric pain, is a host of problems ranging from difficulty in learning to increased risk of chronic illness and mental health issues as an adult. In her case, the pain as not been treated as part of her underlying illness - and dismissed by some of her specialists. And she has become disillusioned and disbelieving that doctors are there to help her. As a former therapist, I almost found myself hoping that my daughter's pain was actually anxiety (hers or mine) and not the patriarchy... however, after a few years of therapy for each of us, lots of investigation of secondary gain, mind-body medicine courses, meditation, and a lot of yoga - our anxiety levels were and are measurably lower while her pain levels and inflammatory markers are higher. During those years of surfing siloed care and "doctor doubts" her oral lesions grew deeper and more painful, her CRP/SED rates steadily climbed, and I continued to push forward to find another answer - working against my own fear that I would be seen as a Munchausen's Mommy Dearest. I also felt deeply that her pain could and should be taken seriously - her pain would leave her sobbing and limp with fatigue; missing birthday parties, trips to the pool, and other coveted childhood moments. It is hard, given the data, for me to believe that this is not tied to the pervasive problem of under-diagnosing and under-treating pain in females and people of color. I would suggest were we turn our attention to research- we would find that female, children of color, are among some of the most under-diagnosed when it comes to pain. That the most vulnerable suffer the most and for the longest. A few weeks ago we met with the Integrated Pediatric Pain and Palliative Care(IP3) Team - a team that sheds light on these and other dynamics around pain to alleviate the suffering of under-treated pain in children. It is the first time anyone on this healing journey has suggested my daughter probably downplays the extremity of her pain and that she has grown accustomed to suffering. She has grown accustomed to be doubted and disbelieved by those charged with her healing. And it is the first time since she became ill that I felt the absence of the patriarchy and racial bias in how her pain was perceived and discussed. She was heard. She was seen. When I imagined being a mom - I imagined picnics on sunny days, glittery tiaras glistening in the light of birthday candles, and sticky hands holding mine while walking to the nearby park. I anticipated patching up skinned knees with colorful bandaids, kissing boo-boo's, and running a cool hand across an occasionally fevered brow. There was no way I could have imagined that one day I would walk into a medical center to sign my 9-year old daughter into a clinical dosing trial for a drug never before used on children. And that I would feel more gratitude and relief than fear and trepidation. This piece has been entered in the Patients Have Power Writing Contest run by Clara Health designed to raise awareness about clinical trials. I am passionate about this cause and hope it will help raise much needed awareness about the power of breakthrough research. That scenario was especially unlikely given my own history as a DES Daughter - a history that includes a drug given to pregnant women that caused catastrophic health problems in the fetuses exposed in utero. As one of those babies born to that legacy I have suffered first hand from drugs not properly, fully, and transparently tested. I also now know what it means when patients have power. When clinical trials are patient-centered and the research transparent. And when informed consent is educated consent. Science has changed since I was born - and I am deeply glad it has. My oldest daughter had a condition that until very recently had no viable cure. As her disease progressed - I found myself having discussions with doctors about teen and young adult years that could include ineffective noxious drugs and organ transplants. I had trepidation about putting my 9-year old in a clinical trial, but total confidence in her research team. Being a clinical dosing trial, she was among the first group of children to ever be researched with this class of drugs. The first day of my oldest daughter's clinical trial was also my youngest daughter's birthday - friends met us at the hospital to cheer on the swallowing of the first dose of trial meds and then joined us at home later that same day to eat birthday cake. That day - we entered the world of clinical trials, biopsies, and birthday cakes. Participation in the clinical dosing trial has ensured that my daughter will live to see and celebrate many years of birthdays.
And while I will always be mindful about the use of any medications with my children - I have experienced first hand the incredible power and promise of emerging research. My daughter is cured. And that is why I am delighted to share our story and to work to support the efforts of www.clarahealth.com to ensure that patients know that they have power. We can and will change the world. I am feeling incredibly grateful for two weeks with "NO" medical appointments - its amazing to suddenly recover the dozens of hours lost weekly to the work of caregiving a sick child. I immediately dove into the list of dozens of neglected areas of my life - starting with the decluttering of the mermaid manor and the finding and hiring of tutors to help the mermaids make up for lessons lost to illness and medical care.
I am so grateful to have small moments; breakfast croissants too burnt to eat accompanied by stories read out loud, mancala duels held on a stacks of overstuffed pillows on the living room floor, walks on warm summer nights with the little dog in jasmine scented air accompanied by the scraping sounds of neighborhood teens skating, pizza picnics on the floor while watching favorite kid movies past bedtime, gathering friends around a backyard fire pit to share stories and s'mores in the flickering shadows of night,, and so much more, I suspect this period will be rife and full of the feelings that got stashed away in the 3-4 year sprint of dealing with the disappearance of the girls' dad, my spine injury, the Commander's illness and clinical trial, Lala's illness and health crises, the mermaid pertussis outbreak, and the relentless spin cycle of illness, worry, the draining of financial reserves to pay for the privilege of surviving these stressors, and the all out effort to work enough hours to keep housing, insurance, and moments of childhood magic intact. I find myself exhausted and grateful. I am so grateful for these moments of normalcy and do not take them for granted. They are among the small moments I imagined when I dreamt of parenting. And after long journeys into the shadow world of childhood illness and the abduction of hope - I fully anchored in living the small moments of those dreams. I am deeply grateful to parent my two girls. Its funny because people always talk about how lucky the girls are that they got me for a mom - but really they should be saying how lucky I am to get to parent my two girls. I am the one who gets the warm hands nestled in mine on crisp walks to school; hugs so hard and sudden I am winded; and lilting voices saying "mama, you got to leave work early". I am deeply grateful for small moments of grace even when it feels like our life is part of a tire fire raging out of control with the horizons obliterated by dark and toxic swirls of never ending waves of smoke. Its one of those periods- both girls are having health stuff.... Its hard to know what is easier to deal with the "we are concerned..." phone calls or the "its probably nothing..." when its clear we are about four days out from an in-patient hospital stay. I know the rhythms of my children and their illnesses well and tomorrow promises to be a hard day medically. I am learning to find grace even in moments when hope is limited. I think, or rather wonder, if this is one of the gifts we parents of sick children are granted- the daily reminders of how lucky we are.
.Yesterday I rode a dharmic boomerang.
I awoke to the news that a beautiful friend had left her body far sooner than any of us imagined; leaving her two young daughters motherless. And by the end of the day; my ten year old daughter had formally said goodbye to the members of the medical research team that had administered life-saving experimental drugs through a clinical dosing trial over the past year. Between those two monumental and life-changing events, I had taken my youngest daughter to urgent care; a visit that resulted in an unexpected and immediate consultation with a pediatric neurologist for the rare and wretched disease that threatens her wellness and tries to steal her health. A disease unrelated to her sister's, evidence that lightening does in fact strike twice, and over and over and over, in the same place. Life and death -- and all the in between -- in the same twelve hours. Only a week and one day earlier - I was graced to hold my friend in my arms one last time and to share our final spoken words. I joined her friends and daughters to love her intensely and with complete focus as she prepared to move from where she lay to enter hospice in the house of her childhood. A home with a garden; magic and healing; a garden her mother still tends. Yesterday, for the first time, I wrapped my arms around my ten year old without the specter of a life-threatening illness shadowing her future. It was a profound moment of catch and release. A moment that is certain to be felt more deeply in the days that follow. As she leaned into the hug and squeezed me tight with arms plump with childhood, I felt graced and overwhelmed with our good fortune. We are outliers of luck of all kinds enveloped by endings and new beginnings. |
AuthorI am mermaid and rebel - a mama to two - I believe in art, music and magic and the rest I cover up with glitter and tattoos. Archives
April 2020
Categories |






 RSS Feed
RSS Feed